From Lab to Life: The Promising Future of Gene Therapy in the War Against Cancer
Gene therapy is emerging as an area of research that may help shape future cancer treatments. Scientists are investigating how genetic techniques could influence the behavior of certain cells, offering new perspectives while highlighting the complexity and ongoing challenges in this field.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
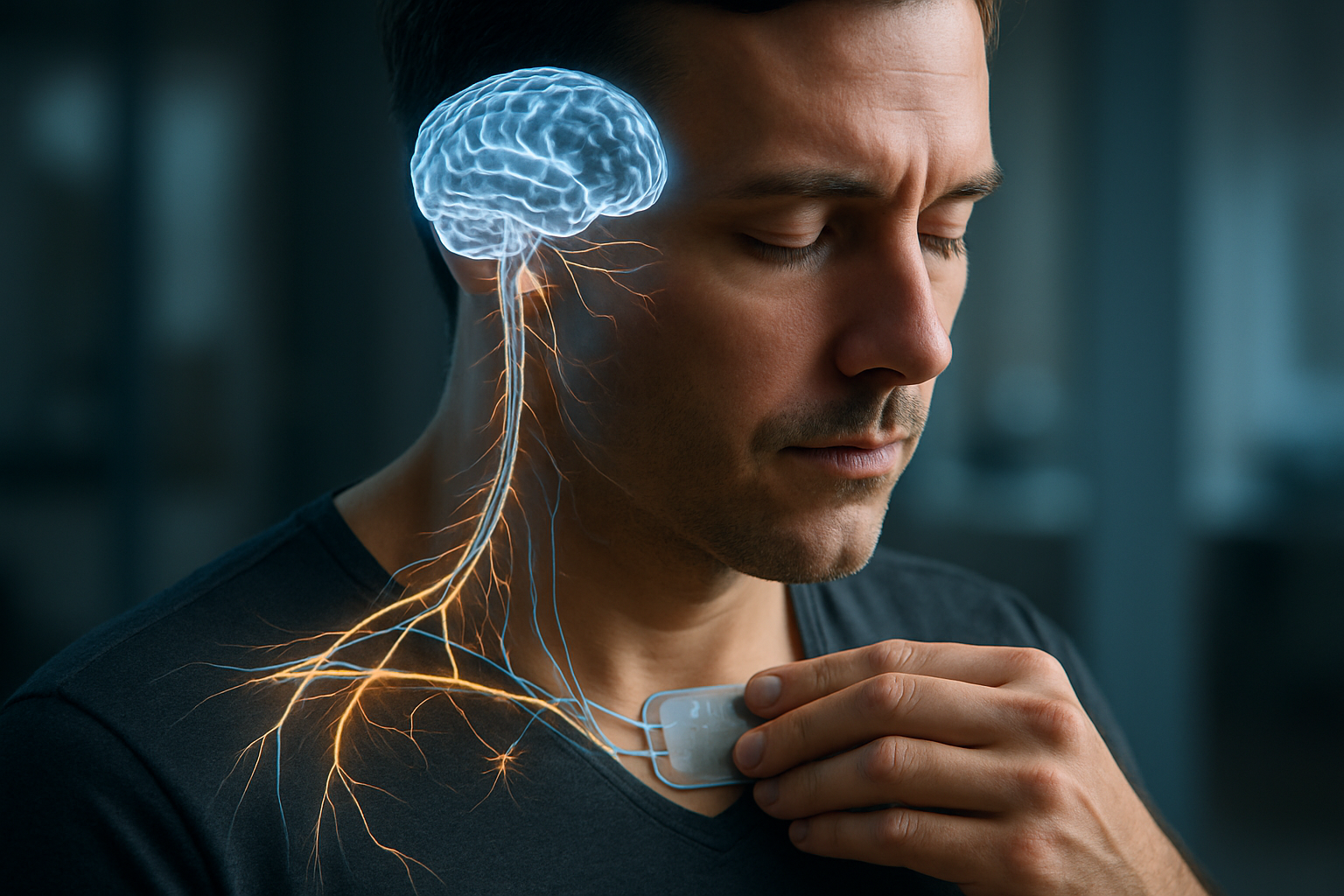
Gene therapy involves altering the genetic material inside a patient’s cells to treat or prevent disease. In the context of cancer, this often means engineering immune cells to better recognize and destroy cancer cells, or introducing genes that can make cancer cells more susceptible to treatment. This complex yet promising field is rapidly evolving, bringing new possibilities to patients who may have exhausted traditional treatment options.
What Are Genetic Therapy Options Available Today?
Several forms of genetic therapy are currently available or in advanced stages of clinical development. One prominent example is CAR T-cell therapy, which involves extracting a patient’s T-cells, genetically modifying them in a lab to produce chimeric antigen receptors (CARs) that bind to specific proteins on cancer cells, and then reinfusing them into the patient. This empowers the immune system to target and eliminate cancer cells more effectively. Other approaches include oncolytic viruses, which are genetically engineered viruses that selectively infect and destroy cancer cells while sparing healthy tissue, and gene editing technologies like CRISPR, which hold potential for correcting specific genetic mutations associated with cancer.
How Do Gene Therapy Clinical Trials Work?
Gene therapy clinical trials are meticulously structured research studies designed to evaluate the safety and efficacy of new genetic treatments. These trials typically proceed through several phases. Phase I trials focus on safety and dosage, often involving a small group of patients. Phase II trials assess efficacy and further evaluate safety in a larger group. Phase III trials compare the new therapy to existing treatments, often involving hundreds or thousands of patients. Participants are closely monitored for adverse effects and treatment response, with ethical oversight and patient safety as paramount concerns throughout the entire process. Strict inclusion and exclusion criteria ensure that participants are suitable candidates for the experimental treatment.
What Genetic Treatment Breakthroughs Have Recently Emerged?
Recent years have seen remarkable breakthroughs in gene therapy, significantly impacting the oncology landscape. The approval of CAR T-cell therapies for certain blood cancers, such as specific types of leukemia and lymphoma, stands as a major milestone. These therapies have demonstrated high response rates in patients with relapsed or refractory disease. Additionally, advancements in gene editing tools, like CRISPR-Cas9, are expanding the potential to precisely correct cancer-driving mutations. Research is also progressing on in-situ gene therapies, where genetic material is delivered directly to tumors within the body, aiming for localized and potent therapeutic effects.
What Does the Future of Gene Therapy Hold?
The future of gene therapy in cancer treatment is anticipated to bring even more sophisticated and personalized approaches. Researchers are exploring ways to make CAR T-cell therapy effective against solid tumors, which present unique challenges due to their complex microenvironments. Efforts are also focused on developing ‘off-the-shelf’ gene therapies using donor cells, which could make treatments more accessible and reduce manufacturing times. Furthermore, the integration of artificial intelligence and machine learning is expected to accelerate the discovery of new gene targets and optimize treatment strategies, leading to more tailored and effective interventions for individual patients. The development of combination therapies, pairing gene therapy with other treatments like immunotherapy or chemotherapy, also holds significant promise.
How Are Gene Therapy Advancements Changing Treatment Landscapes?
Gene therapy advancements are fundamentally reshaping the paradigm of cancer treatment, shifting it towards more targeted and potentially curative interventions. For patients with specific types of advanced cancers, these therapies offer a chance for long-term remission, sometimes even after conventional treatments have failed. This has led to a re-evaluation of treatment algorithms and an increased focus on precision medicine. While these therapies are complex and carry their own set of considerations, their success underscores a transformative shift in oncology, moving from broad-spectrum treatments to highly specific, biologically driven approaches that harness the body’s own mechanisms to fight disease.
Gene therapy treatments are highly specialized and vary significantly in cost depending on the specific therapy, the patient’s condition, the healthcare provider, and geographic location. The following table provides general cost estimations for some types of gene therapy, but these figures can fluctuate widely.
| Product/Service | Provider Category | Cost Estimation (USD) |
|---|---|---|
| CAR T-cell Therapy (e.g., Kymriah) | Specialized Cancer Centers | $375,000 - $475,000 |
| CAR T-cell Therapy (e.g., Yescarta) | Specialized Cancer Centers | $375,000 - $450,000 |
| Gene Editing Research Therapies | Research Institutions | Highly Variable |
| Viral Vector Gene Delivery | Research Institutions | Highly Variable |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Gene therapy represents a monumental leap forward in medical science, offering profound implications for cancer treatment. While still an evolving field, its ability to address diseases at a genetic level provides a compelling vision for future medicine. Continued research and clinical innovation are vital to expanding the reach and efficacy of these life-changing therapies, ultimately offering new avenues of hope for countless patients facing challenging diagnoses.




