Early Indicators of Liver Cirrhosis in the United States 2025: Signs to Notice and When to Seek Medical Help
Liver cirrhosis often develops silently in early stages. Recognizing early warning signs is crucial, especially for adults over 45 or those with risk factors. This article outlines common early symptoms of cirrhosis, possible complications, and guidance on when to seek medical care in the United States (2025).
Understanding Liver Cirrhosis and Why It Matters
Liver cirrhosis is a serious illness characterized by permanent scarring of liver tissue caused by prolonged inflammation and damage. This scarring limits the liver’s ability to function properly, disrupting its essential roles such as detoxifying the blood, processing nutrients, producing bile, and supporting blood clotting. Cirrhosis generally develops over time and, if left untreated, may result in liver failure or liver cancer.
In the United States, cirrhosis affects about 0.25% of the adult population overall; however, this prevalence nearly doubles among adults aged 45 to 54. It ranks as a leading cause of liver-related hospitalizations and deaths, with approximately 26,000 fatalities each year due to the condition. Since the liver is resilient and compensates for damage in the early stages, many individuals remain unaware they have cirrhosis until symptoms worsen.
Early Phase: The Silent Stage of Cirrhosis (Compensated Cirrhosis)
During the early or compensated phase, the liver continues to perform most of its functions despite some scarring. Many people experience no symptoms in this stage. For this reason, routine health screenings and medical evaluations are particularly important, especially for those at risk. Detecting cirrhosis early opens the door to interventions that can slow the disease’s progression.
Subtle Early Signs to Notice
When symptoms do appear, they tend to be mild and easy to overlook, including:
- Ongoing fatigue or weakness
- Loss of appetite or unintentional weight loss
- Mild abdominal discomfort or a feeling of fullness
- Slight swelling or bloating
While these signs alone are not definitive for cirrhosis, they deserve medical assessment if they persist alongside risk factors such as chronic alcohol use, chronic viral hepatitis (B, C, or D), metabolic disorders like obesity or type 2 diabetes, or a family history of liver disease.
Advancing Symptoms: Decompensated Cirrhosis
As liver damage worsens, more pronounced and serious symptoms emerge, indicating decompensated cirrhosis. These symptoms demand expedited medical evaluation and can include:
- Jaundice: Yellowing of the skin and eyes caused by bile accumulation
- Ascites: Abdominal swelling due to fluid buildup
- Easy bruising or bleeding owing to impaired clotting
- Confusion, memory issues, or drowsiness linked to hepatic encephalopathy (brain dysfunction caused by liver failure)
- Gastrointestinal bleeding, often recognizable by vomiting blood or black, tarry stools
These symptoms show the liver is failing to maintain its functions and complications such as portal hypertension (high blood pressure in the liver’s blood vessels) have developed.
Critical Signs Warranting Immediate Medical Attention
Certain symptoms signal potentially life-threatening complications requiring urgent intervention:
- Sudden, intense abdominal pain
- Vomiting blood
- Black or tarry stools indicative of internal bleeding
- Serious confusion or loss of consciousness
- Rapidly worsening swelling in the abdomen or legs
These signs may point to severe bleeding from varices (enlarged veins), liver failure, or encephalopathy. Emergency medical care is essential in these situations.
Who Should Exercise Extra Caution?
Certain groups within the United States face a higher risk and should closely monitor their liver health:
- People with chronic alcohol use disorder
- Individuals with chronic hepatitis B, C, or D infections
- Those with metabolic syndrome traits, such as obesity and type 2 diabetes
- People with a family history of liver disorders
- Patients with bile duct conditions or genetic diseases like hemochromatosis or Wilson disease
For these populations, regular medical checkups including liver function assessments and imaging are strongly advised, even if no symptoms are present.
Preventing Cirrhosis Progression via Early Detection and Lifestyle Adjustments
Detecting liver disease early, before cirrhosis develops, is critical. Vaccinations for hepatitis B and lifestyle changes—such as limiting alcohol consumption, managing diabetes and obesity, and avoiding liver toxins—can help prevent or slow progression.
If liver disease is identified early through blood work, imaging, or biopsy, healthcare providers in the United States can act to manage the underlying cause, reduce inflammation, and minimize permanent damage.
How Is Liver Cirrhosis Diagnosed?
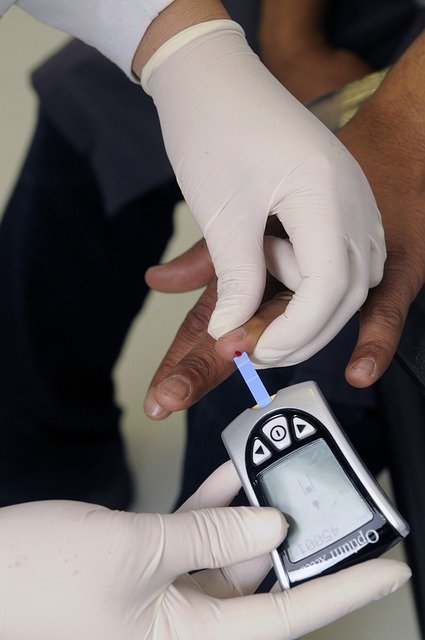
Diagnosis begins with a review of symptoms and medical history, including alcohol and medication use. Physical examinations focus on signs like jaundice, abdominal swelling, and unexplained bruising.
Tests frequently employed include:
- Blood tests to assess liver enzymes and function
- Imaging techniques like ultrasound and elastography to evaluate liver stiffness and scar tissue
- Liver biopsy when diagnosis or assessment of severity is unclear
These diagnostic tools assist in planning treatment and determining prognosis.
Treating Cirrhosis and Its Related Complications
Although cirrhosis cannot undo existing liver scarring, treatments aim to:
- Treat the root causes via antiviral drugs, control of metabolic syndrome, or cessation of alcohol
- Manage symptoms and complications such as ascites and hepatic encephalopathy
- Prevent life-threatening events like variceal bleeding through medication or procedures
- Monitor regularly for liver cancer development
Ongoing medical care improves both quality of life and survival rates.
When Is a Liver Transplant Needed?
For advanced cirrhosis accompanied by signs of liver failure or severe complications unresponsive to treatment, liver transplantation may be considered. Patients with decompensated cirrhosis typically receive priority on transplant waiting lists.
Evaluation involves reviewing overall health, disease stage, and transplant eligibility. This procedure can provide a life-saving alternative for those with end-stage liver disease.
The Value of Routine Liver Health Screening
Since liver diseases often show no symptoms until advanced stages, regular liver health assessments are essential. Adults over 45 or those with risk factors should discuss liver screening with their doctors during routine visits.
Early testing allows detection of liver abnormalities before cirrhosis onset, enabling timely interventions through lifestyle changes or medical treatments to safeguard liver function.
Being aware of early signs and risk factors of liver cirrhosis empowers individuals in the United States to promptly seek medical care and engage in preventive strategies. In 2025, continued progress in diagnosis and treatment is enhancing outcomes for those living with liver disease.
Sources
- Cleveland Clinic: Cirrhosis of the Liver
- American Liver Foundation: Cirrhosis of the Liver
- National Institutes of Health: Consider Your Liver (2025)
Disclaimer: This article provides general health information and does not replace professional medical advice. If you experience symptoms or suspect you may be at risk for liver disease, please consult a healthcare professional for personalized evaluation and care.




